Medical Screening Process for Prospective Donors Explained
Becoming a sperm donor involves comprehensive medical evaluations designed to ensure the health and viability of donations. This rigorous screening process protects both recipients and donors while maintaining the highest standards of reproductive healthcare. The evaluation encompasses physical examinations, genetic testing, psychological assessments, and ongoing health monitoring throughout the donation period.
The journey to becoming a sperm donor begins with an extensive medical screening process that can take several months to complete. Fertility clinics and sperm banks maintain strict protocols to ensure only the healthiest candidates are accepted into their programs. This comprehensive evaluation protects the health of future children, recipients, and donors themselves.
Understanding Sperm Donation Requirements
Medical screening starts with basic eligibility criteria that vary by facility but generally include age requirements between 18 and 39 years old, height and weight specifications, and educational background verification. Candidates must demonstrate good physical and mental health, with no history of genetic disorders or sexually transmitted infections. The initial application process involves detailed questionnaires about family medical history, lifestyle habits, and personal health records.
Physical examinations include comprehensive blood work, urine analysis, and genetic testing for inherited conditions. Clinics screen for chromosomal abnormalities, cystic fibrosis, sickle cell disease, and other hereditary disorders. Psychological evaluations assess mental health stability and ensure candidates understand the emotional implications of donation.
Paid Sperm Donation Compensation Structure
Compensation for sperm donation varies significantly based on location, clinic policies, and local regulations. In the United States, donors typically receive between $35 to $125 per acceptable donation, with most clinics paying around $70 per sample. European facilities often offer lower compensation due to different regulatory frameworks, ranging from €25 to €75 per donation.
The payment structure usually includes base compensation plus bonuses for meeting quality standards and consistency requirements. Some facilities offer additional payments for donors who complete extended commitment periods or possess rare genetic profiles. However, compensation should never be the primary motivation for donation, as the screening process eliminates many applicants.
| Facility Type | Average Payment per Donation | Additional Benefits |
|---|---|---|
| Major US Sperm Banks | $70-$125 | Health screenings, genetic counseling |
| University Programs | $35-$75 | Research participation opportunities |
| European Clinics | €25-€75 | Limited compensation due to regulations |
| Private Fertility Centers | $50-$100 | Flexible scheduling, premium programs |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
Who Can Become a Sperm Donor
Eligibility requirements extend beyond basic health criteria to include lifestyle factors and commitment levels. Successful candidates typically maintain healthy lifestyles, avoid smoking and excessive alcohol consumption, and can commit to regular donations for 6-12 months. Educational backgrounds often require high school completion, with many programs preferring college-educated donors.
Age restrictions exist because sperm quality typically declines after age 40, though some facilities accept donors up to 45 years old. Height requirements usually mandate donors be at least 5’7” tall, reflecting recipient preferences rather than medical necessity. Weight restrictions ensure donors maintain healthy BMI levels throughout the donation period.
Genetic diversity considerations mean facilities actively seek donors from various ethnic backgrounds to serve diverse recipient populations. Some programs specifically recruit donors with rare genetic profiles or unique physical characteristics to meet specific recipient requests.
Medical Testing and Health Monitoring
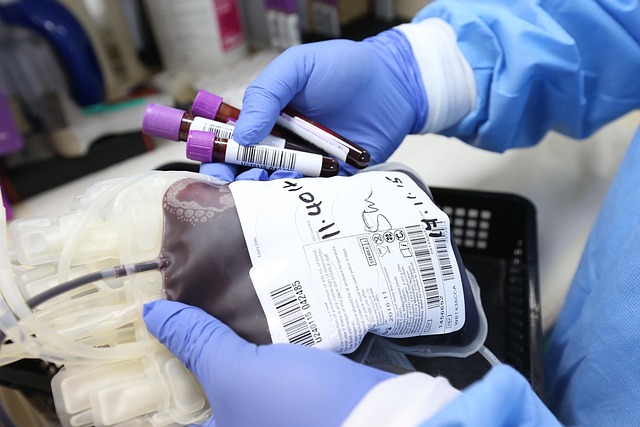
The screening process includes extensive laboratory testing performed at regular intervals. Initial testing covers sexually transmitted infections including HIV, hepatitis B and C, syphilis, gonorrhea, and chlamydia. Genetic testing examines chromosomal structure and screens for over 100 hereditary conditions.
Sperm quality analysis evaluates concentration, motility, and morphology to ensure samples meet strict standards for freezing and storage. Donors must provide multiple samples over several weeks to establish consistent quality patterns. Any sample failing to meet minimum standards results in rejection of that donation.
Ongoing monitoring continues throughout the donation period with quarterly STI testing and annual comprehensive health evaluations. Donors must report any changes in health status, medication use, or lifestyle factors that could affect sample quality or safety.
Psychological and Social Considerations
Psychological screening evaluates candidates’ understanding of donation implications and their ability to handle potential future contact from offspring. Counseling sessions discuss anonymity policies, legal rights and responsibilities, and emotional aspects of genetic parenthood.
Many facilities require psychological evaluations by licensed mental health professionals who specialize in reproductive medicine. These assessments identify candidates who may struggle with the emotional aspects of donation or have unrealistic expectations about the process.
Social considerations include relationship status discussions and partner consent when applicable. Some programs require written consent from spouses or long-term partners, acknowledging their understanding and support of the donation decision.
The medical screening process for sperm donation represents one of the most comprehensive health evaluations available, often detecting health issues donors were previously unaware of. This thorough approach ensures the safety and success of assisted reproductive treatments while maintaining the highest standards of medical care for all parties involved.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




